For most women, pregnancy is a time of anticipation and change. Emotions of joy and anxiety collide as hormone levels increase to accommodate new life. But, for some women, the fear of miscarriage is ever-present.
Statistically, “among women who know they are pregnant, the miscarriage rate is roughly 10-20%, while rates among all fertilization is around 30% to 50%.”1 Almost everyone knows someone who has been through miscarriage and its devastation. Although we struggle to find the right words, we usually end up saying things that are not at all helpful in easing the grief felt by the family.
Risk factors for miscarriage, usually occurring in the first trimester, include advanced maternal age, previous miscarriage, exposure to tobacco smoke, obesity, diabetes, thyroid problems, and drug or alcohol use. In fact, for women over the age of 40, the risk of miscarriage can be as high as 45%.1
Once a pregnancy has progressed to the second trimester, the most likely cause for miscarriage is related to cervical insufficiency, sometimes called an incompetent cervix. This condition can be “congenital or acquired...The most common acquired cause is cervical trauma, such as cervical lacerations during childbirth, cervical conization, LEEP (loop electrosurgical excision procedure), or forced cervical dilatation during the uterine evacuation in the first or second trimester of pregnancy.” 2 While these conditions only occur in <1% of the obstetric population, the hope felt by the family increases each day that the pregnancy remains viable.
While many women would prefer to use conservative means of treatment for incompetent cervix like limiting activity, bedrest, and pelvic rest, they “have not proven effective and their use is discouraged.”3 One treatment for incompetent cervix that has been shown to be successful in prolonging pregnancy is the cervical cerclage procedure. This procedure uses suture to stitch the cervix closed, either as a proactive step early in the pregnancy (called elective cerclage), or as an emergent step in an already dilating cervix. Recent research shows us that after cerclage was placed in women with a previous preterm delivery, 69% of the successive pregnancies delivered at term (>37 weeks), and 17% delivered between 28-37 weeks.3 In general, with a singleton pregnancy, the “success rate for cervical cerclage is approximately 80-90% for elective cerclages, and 40-60% for emergency cerclages.”4
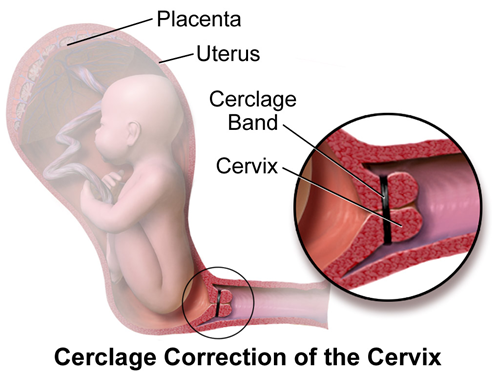
Source: Blausen Medical Communications
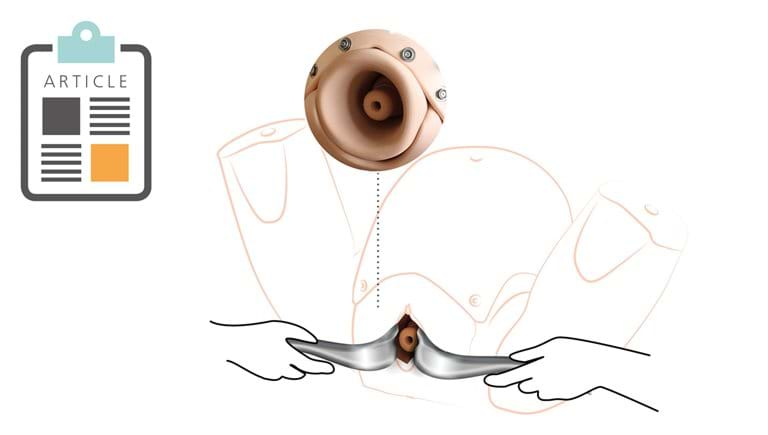
Two leading obstetric experts, Dr. Graham Tydeman, Consultant Obstetrician & Inventor, NHS Fife, and Professor Andrew Shennan OBE, Consultant Obstetrician and Director of the Clinical Trials Unit in the Women’s Academic Health Centre, partnered with the Limbs & Things development team to create a realistic training solution for cervical cerclage.
Dr. Tydeman and Prof. Shennan OBE, use the PROMPT Flex Birthing Simulator for teaching and training, and have rigorously tested the module to ensure it meets the standards needed to teach and maintain the skill of cervical cerclage. The new PROMPT Flex Cervical Cerclage module is the latest development in our ever-evolving commitment to healthy moms and babies. Encouraging the provider to practice both elective and emergent procedures in a controlled environment will build not only competence, but also confidence in their ability to deliver safe care during a stressful time for the patient and her family.
1: Miscarriage
2: Cervical Incompetence
3: Success Rate of Cervical Cerclage in preventing Preterm Labour
4: Cervical Cerclage